The liver is fatty without alcohol consumption
NAFLD the global concern
17 Oct 2024 | Chin
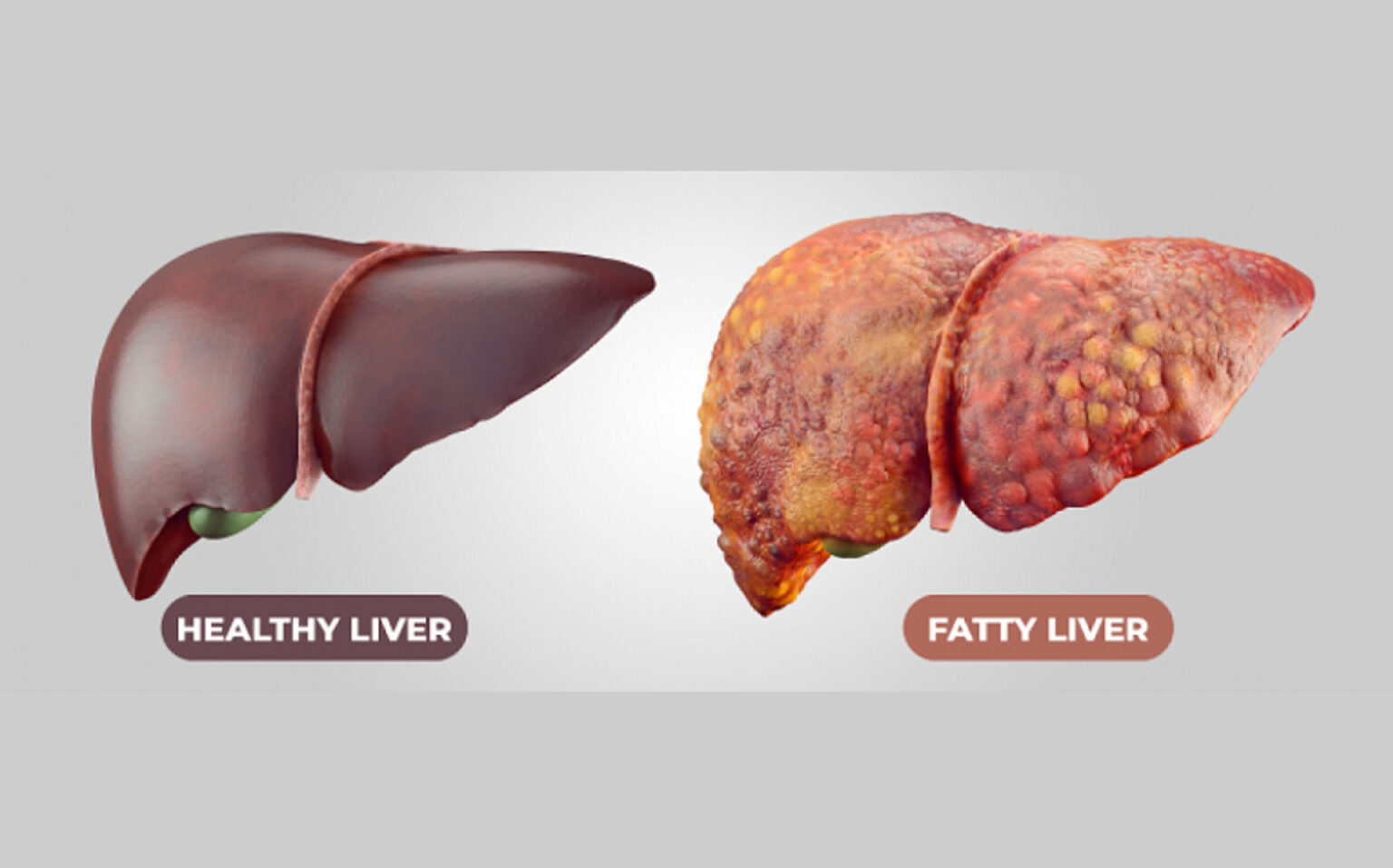
Non-alcoholic fatty liver disease (NAFLD) is a condition where fat builds up in the liver, unrelated to alcohol consumption. When 5-10% of liver weight is made up of fat, inflammation occurs, leading to NAFLD. It is the most common cause of liver disease globally, with a prevalence of 25-27% in Asia. In Malaysia, 23% of the general population and 49.6% of diabetic patients suffer from NAFLD, and the rate goes up to 90% in obese individuals. NAFLD, if left untreated, can progress to nonalcoholic steatohepatitis (NASH), a more severe form that causes liver inflammation and damage. Early detection and intervention are key to preventing this progression and avoiding complications like cirrhosis or liver cancer.
Causes of NAFLD
NAFLD forms without alcohol due to several factors:
- Insulin Resistance: Insulin resistance impairs the body’s ability to regulate fat metabolism, leading to an increased delivery of fatty acids to the liver. When cells fail to respond to insulin, excess glucose gets converted into fat, resulting in fat deposits in the liver.
- Obesity: Excess weight, particularly visceral fat, promotes fat accumulation in the liver. This explains why NAFLD is more prevalent in obese individuals, with up to 90% of them affected.
- High Sugar Diets: Diets rich in refined carbohydrates and sugars cause the liver to convert unused glucose into fat, leading to liver fat accumulation. Glycogen storage becomes overwhelmed, causing fat buildup.
- Metabolic Syndrome: Conditions like high blood pressure, abnormal cholesterol levels, and high blood sugar, which are often present in metabolic syndrome, increase the risk of NAFLD.
- Genetic Factors: Certain genetic predispositions make some people more susceptible to storing fat in their liver, increasing their likelihood of developing NAFLD.
View the video for more information on how NAFLD forms
Diagnosis of NAFLD
Diagnosing NAFLD involves several methods, including:
- Liver Enzyme Tests: Elevated liver enzymes, particularly ALT and AST, may indicate liver inflammation caused by NAFLD. However, enzyme levels are not always indicative of disease severity.
- Imaging Techniques: Ultrasound, CT scan, or MRI can detect liver fat accumulation. Ultrasound is the most used imaging method, though it cannot assess inflammation or fibrosis.
- FibroScan (Transient Elastography): This specialized ultrasound measures liver stiffness, which can indicate fibrosis or scarring. It helps assess the progression from NAFLD to more severe conditions like nonalcoholic steatohepatitis (NASH).
- Liver Biopsy: The gold standard for confirming NAFLD and differentiating it from NASH. A small sample of liver tissue is examined under a microscope to evaluate inflammation, fat accumulation, and fibrosis.
- Blood Tests and Biomarkers: Several blood tests and biomarker panels can provide an estimate of liver fat content and fibrosis without requiring a biopsy.
Treatment and Interventions
- Weight Loss and Diet: The primary treatment for NAFLD is lifestyle modification. Losing 7-10% of body weight through diet and exercise can significantly reduce liver fat and inflammation. A diet low in refined sugars and saturated fats is recommended.
- Exercise: Regular physical activity helps improve insulin sensitivity and reduce fat buildup in the liver. Even moderate exercise, like walking or cycling, can make a difference.
- Medications: While no specific drug is approved for treating NAFLD, medications targeting insulin resistance and blood glucose management, such as metformin, or anti-inflammatory agents like vitamin E, may be used to manage the condition.
- Management of Underlying Conditions: Controlling diabetes, high blood pressure, and high cholesterol is essential to prevent the progression of NAFLD. Medications like statins or anti-diabetics may be prescribed.
- Surgery for Obesity (Bariatric Surgery): In cases of severe obesity, bariatric surgery has been shown to reduce liver fat and improve NAFLD outcomes by promoting significant weight loss.
What we have in Goodness Through Food?
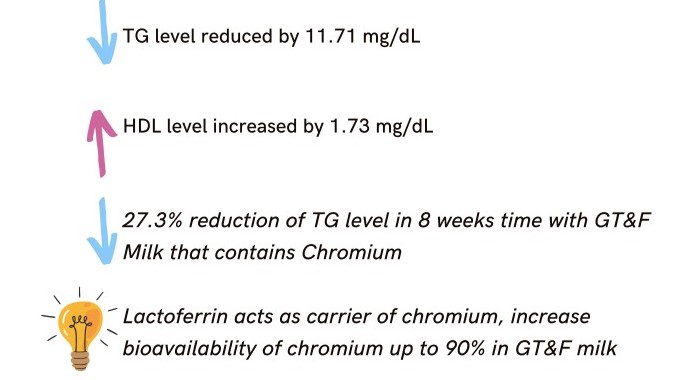
GTF Chromium improves insulin sensitivity, helping regulate blood glucose and fat metabolism. By reducing sugar and fat in the liver, it provides hepaprotective effects by lowers triglycerides and LDL, reduces inflammation, and rejuvenates cells.
Benefits of GTF Chromium for Liver Health
GTF Worldwide Sdn Bhd
- No. 20-2, Plaza Danau 2, Jalan 5/109F, Taman Danau Desa, 58100 Taman Desa, Kuala Lumpur, Malaysia.
- (03) 7982 9881
- (012) 483 5523
- info@gtf.com.my